The new 39-bed Neonatal Intensive Care Unit (NICU) at Beacon Children’s Hospital in South Bend, Ind., features enhanced single-family rooms (SFR) and couplet care rooms (CCR), two new room designs that expand clinical functionality and family accommodation in the NICU. The hospital’s NICU staff holds the conviction that babies belong with their parents whenever possible, and desired to make this practice available not only in the SFRs but also for postpartum mothers who are still patients. Previously, some mildly ill or premature babies were taken to the mother’s postpartum room to accomplish this, but most babies were not eligible due to the severity of their illness. Both types of rooms in the new NICU are designed to accommodate mothers who are still patients immediately after birth. This facilitates early bonding between mother and child, which historically has been limited during the first few days of a NICU baby’s life.
NICU design is evolving in response to research that babies will have better health and developmental outcomes if their physical surroundings support new care models, such as couplet care, skin-to-skin care, and family-centered/integrated care. Many studies show the benefits of skin-to-skin in their mother’s arms, or “kangaroo care,” for babies in the NICU, because it is comforting and helps newborns adapt to life outside the womb. Couplet care, which promotes family bonding by allowing mother and newborn to stay together while in the hospital, and family-centered/integrated care, where parents are included as part of the care team, are driving the need for newly designed space to accommodate families in the NICU.
The high-intensity NICU can be a very stressful place for babies. Conventional open-ward NICU’s have an inappropriate sensory environment for infants, with noise levels from alarms and activities that impair the infant’s ability to sleep, develop, and grow. The open environment is also stressful for families: The lack of space, privacy, and control make extended time in the NICU uncomfortable, creating a barrier for parents to spend time in extended intimate contact with their baby.
Research shows that SFRs support longer parental stays and improve infant outcomes with reduced length of hospitalization. The new SFRs at Beacon Children’s have several elements that promote improved sensory development for the baby and family participation in care, including a family area with a toilet room and shower within each room. A sliding frosted glass door separates this area from the rest of the room, providing privacy and quiet at night.
Every NICU room has a window to provide a sense of normalcy by connecting to daily cycles of light. Because views of nature can also reduce stress and provide positive distraction for parents who may be distraught or depressed, an innovative feature of the Beacon Children’s NICU is an interior courtyard visible from the rooms.
All lighting in the room is dimmable for families to control the light levels. No lights are located directly over the baby’s bed, so there is no chance of direct light shining into the baby’s eyes. The procedure light is instead mounted on an adjustable arm. Colored LEDs at the footwall wash the wall with color to personalize the room. The color can easily be changed to vary the experience in the room and to suit the mood from day to day. Wall sconces in the family area provide a soft level of light for reading or conversation.
Multiple Configurations Possible
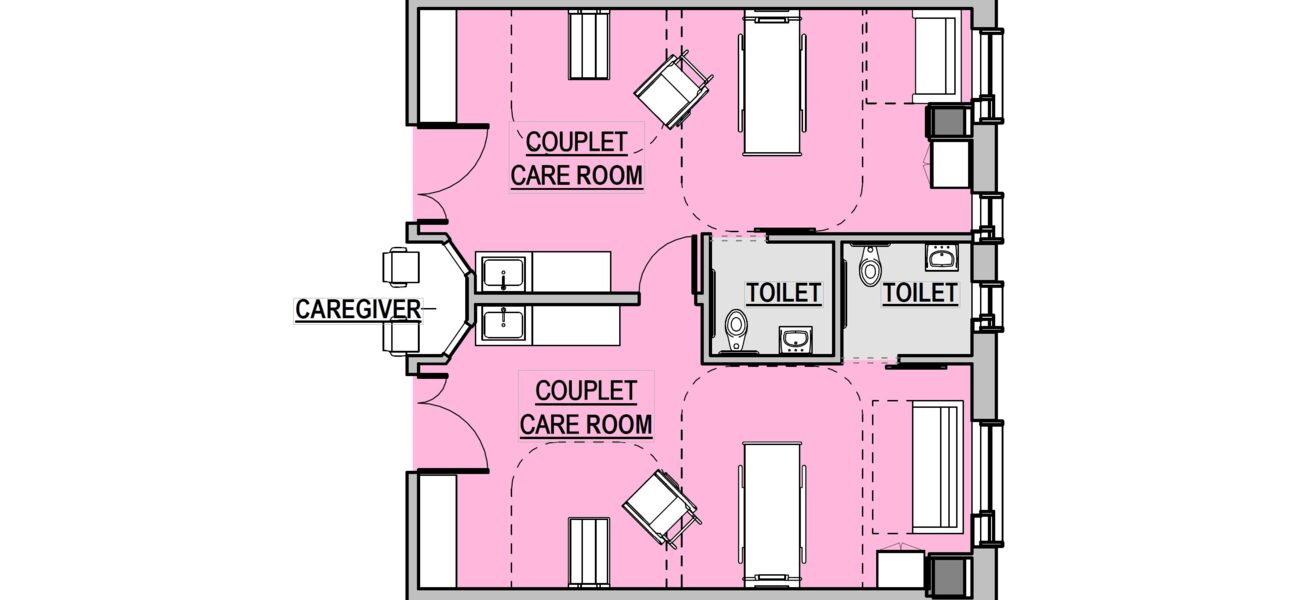
Couplet care rooms are modeled after those in Sweden’s University Hospital of Karolinska, where the rooms accommodate the entire family unit. The CCR has many of the same features of the SFR but with a second headwall for the mother’s bed, including the code-required clearances around the bed. Beacon Children’s Hospital has expanded the functionality of the CCR to accommodate multiple babies, group care, and other care scenarios, giving the NICU increased flexibility.
When a CCR is paired with an SFR or another CCR, it can accommodate a mother with twins or higher-order multiples. A door in the sidewall provides easy access between the rooms. Each headwall can serve one critical baby or two intermediate babies. Kangaroo chairs allow both parents to provide skin-to-skin care for their babies together.
While the SFR provides an ideal environment for families, it can become an isolation room for babies whose families rarely visit. In those instances, the larger rooms support group care by providing roommates for babies, which facilitates more frequent interactions with nursing staff.
The additional space in the CCR also accommodates “super-critical” babies who need much more equipment and larger teams to provide specialized care. The CCR’s larger size provides the space needed to perform procedures if an infant requires surgery.
Lastly, families need space and privacy to be with their baby during hospice care. Larger groups of family members often will come to spend time with the baby, and a pair of connected CCRs can provide the additional accommodation needed to support the family.
After being in the new space, the staff found that some parents began to treat their room more like a hotel and were declining room service for the day. For infection control purposes, Beacon Children’s staff inform parents that they need to be awake and have the parent space in the room picked up and ready for housekeeping by 9 a.m. each day. Setting this expectation on admission, and explaining that this is to help prevent an infection for their baby, has been very effective. Children’s has also changed its policy to allow food in all rooms on the unit, while setting the expectation for cleanliness to prevent the risk of infection.
Experience gained during limited couplet care in the old NICU was extremely valuable in obtaining buy-in from obstetricians, postpartum nurses, administration, and nursing staff, all of whom saw first-hand how beneficial couplet care is for families. While the CCR enhances patient outcomes and the patient family experience, the novel design also impacts the training and assignments of nurses, so that they can achieve the model of care supported by this room design.
A core group of nurses in the NICU are trained to provide care for both postpartum mothers and NICU babies up to an intermediate care level. Nurses who provide couplet care in the NICU complete both postpartum and NICU skills validations on an annual basis, which was not required with the more traditional NICU design. A new scope of service was established for postpartum mothers cared for in the CCRs. All attempts are made to care for the mother and baby as a couplet assignment, but they may have separate nurses when the medical needs of the baby are more critical.
Lessons Learned and Outcomes
The lessons learned from Beacon Children’s NICU unit can be applied to any health system considering a NICU redesign:
- Know the research and evidence: For Beacon Children’s, this was critical in helping administration, staff, and other stakeholders understand the benefits and potential outcomes. During planning, integrated design events were held to provide hands-on participation by staff and families to test the prototype, using iterative, full-scale mock-ups and simulations to ensure that functional and code requirements were met.
- Incorporate couplet care however possible: Research has shown that couplet care supports improved developmental outcomes for newborns and improved quality of life as they mature into adults.
- Project utilization of the two room types as accurately as possible to get the right proportion of each.
The new Beacon Children’s NICU has already provided positive outcomes. The average length of stay has decreased by 1.7 days since introducing couplet care in the NICU, and patient satisfaction scores average 4.7 on a 5-point scale. Additionally, the environment of the new unit has had an overall positive impact on staff satisfaction. Most notable is the exposure to natural light they have from the windows, atrium, and outdoor garden.
By Sue Ann Barton, AIA, LEED AP BD+C, EDAC; and Jennifer Tonkovich
Sue Ann Barton is a principal in the Portland, Ore., office of ZGF Architects LLP; Jennifer Tonkovich is the director of children’s services at Beacon Children’s Hospital in in South Bend, Ind.