More and more universities are building their scientific research centers around cores of huge, heavy, yet surprisingly delicate equipment. Building a core laboratory facility forces architects and campus planners to think about logistics, timing, and backup systems to a level of detail probably more familiar to NASA engineers than institutional architects. As the team behind Emory University’s new Health Sciences Research Building II (HSRB-II) learned, a huge range of factors—in their case, everything from the amount of rebar in the flooring to the width of the corridors to shipping velocity on the Suez Canal—must be reckoned with before such a facility is completed.
In certain respects, the challenge may be even greater than the kind typically faced by rocket scientists. Although the concept of the core laboratory facility is simple—bringing a lot of powerful hardware together creates economies of scale and attracts talented researchers—designing and building a core facility is extremely complex.
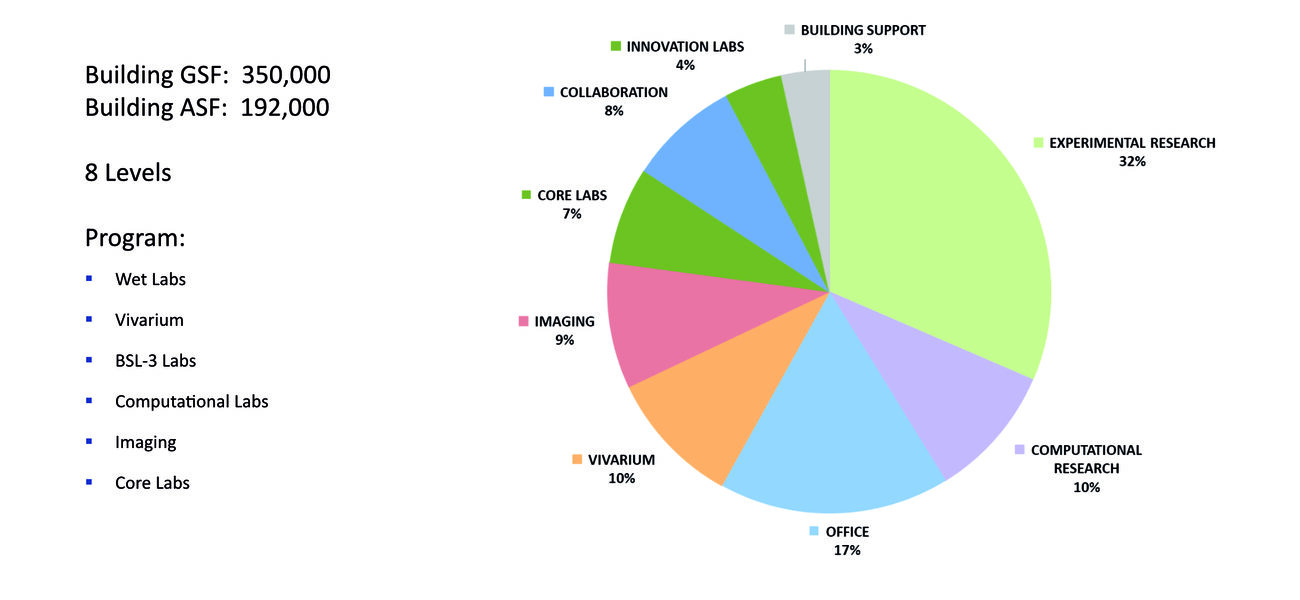
“We had to understand how the different pieces of equipment worked together,” explains Ellen Ignacio, senior associate and senior lab planner for HOK, which designed the Atlanta university’s new 350,000-gsf building and managed its construction. “Even though the different pieces of equipment might not necessarily operate together, they all had shielding requirements; they had infrastructure, conduit, and power requirements; and all these things needed to be defined and coordinated with the design and sequence of construction.”
The project began with strategic master planning in 2016, a feasibility study in 2017, detailed programming and architectural design work in 2018, followed by construction, which continued up to its commissioning in 2023.
Preparing for the Electric Tenants
Divided into wet labs, a vivarium, BSL-3 labs, computational labs, imaging labs, core labs, and innovation labs, the eight-level, $288 million building would play a central role in the work of over 1,000 researchers in pediatrics, biomedical engineering, oncology, cardiovascular medicine, vaccines, radiology, and brain health. The building would also house $25 million worth of high-demand research equipment, some of it weighing thousands of pounds, and much of it fragile or sensitive.
In all, 20 different core facilities needed to be consolidated into the new building: biostatistics, cytometry, integrated computation, proteomics, stem cells, investigational drug services, rodent behavior, systems imaging, glycomics and molecular interactions, integrated genomics, multiplexed immunoassay, bioanalytics, mouse transgenic and gene targeting, integrated biorepository, animal resources, gnotobiotic animals, integrated metabolomics and lipidomics, cellular and immunotherapy, integrated cellular imagry, and advanced electron microscopy.
“Every single manufacturer had a different version of site readiness that was required for their equipment,” says Chirag Mistry, senior principal and regional leader for science and technology at HOK. “Some needed a secure data connection, some needed continuous chilled water, and some had other requirements. The design team and the owner had to put it in simple English so that the contractor would understand what things we needed to have in place before the equipment arrived.”
Most equipment also needed a stable internet connection during construction, as machines had to be able to not only communicate to the vendor but also to receive instructions back. Other machines had to link with each other when they had not been designed to connect, such as equipment designed in the Netherlands and built on metric measurements that had to connect to an American system built on the Imperial standard, over conduits that had a tolerance of only millimeters.
The design of the facility itself also depended in large part on the equipment requirements, which dictated the floor-to-floor height, the amount of structural support needed, the mechanical and electrical systems, the amount of rebar in the slab, and other details, adds Mistry.
Core Principles
Looking back now on the four-plus turbulent years it took to build the new core facility, the team that managed the design of the building has several suggestions to offer the growing number of campus planners who face a similar challenge.
At the top of Mistry’s list: Ask the research teams to decide on the equipment they want to buy as early as possible, and if they can, to get purchase orders issued on all that equipment.
An early decision matters because vendors often don’t like to share detailed plans of the equipment before there is a purchase order in place. However, without such plans, it’s difficult for the architectural team to create the right space, including connections to the right utilities and redundant systems, and big enough corridors to move the equipment into place. Such equipment is often massive: A cyclotron can weigh 40,000-50,000 pounds, for example, or an MRI scanner 60,000 pounds, according to Mistry.
It’s also useful to know something about the governance of the machine, advises Mistry. “How is this equipment going to be managed? Who is going to run it? How is it going to be accessed?” All this information is critical to establishing a final design solution.
After collecting the basic specifications, ongoing communication is crucial. For the HSRB-II, Emory’s architecture and lab planning team held weekly calls with equipment vendors to ensure that manufacturing, shipping, and delivery were all on track.
“What I’ve learned over time is that things are going to happen. It’s not if; it’s when. It’s how we deal with those issues when they arrive that makes all the difference,” says Melissa Thackery, former program manager for Emory. “We had COVID in the middle of the project. We came together as a team and we came to the table with solutions. We didn’t just throw our hands up in the air and say it is somebody else’s problem.”
“You have to get to a certain point in your construction, you have to deliver the thing, and then you have to finish building around it,” she says. “For instance, the cyclotron had to have a leave-out in the 12-inch-thick concrete vault wall; we couldn’t build that until it arrived. When you have a cyclotron vault, you have to have a door to get in and out, and it has to be filled with lead bricks—an 11,000 pound door!”
University counsel, insurers, and public safety authorities also had to be consulted during the installation of the equipment in the HSRB-II. “If you have a 7-Tesla MRI on an active construction site, you can’t just walk into the room, because the magnetic field will affect a heart pacemaker if you have one,” says Thackery.
Several consulting teams participated in those calls, including the equipment manufacturers and JE Dunn Construction, the construction manager. “We were often working with four or five different time zones and multiple equipment manufacturers, trying to get them to coordinate among themselves and the design engineers and construction partners. It literally took a village to bring together all of these equipment pieces in the building,” says Mistry.
Some equipment needed to be designed with different access points, to share equipment between different types of uses. For one imaging machine that would be used for animals and by humans, the team designed a dual corridor system in which people would enter and exit from the left and animals from the right.
The building design itself needed to reflect the needs of the equipment, with special requirements satisfied, such as low-vibration floors and quench vents, and floors with a surveyor-certified degree of flatness.
Large imaging equipment was sent to the first basement and small imaging equipment to the second floor, with two spare rooms for future additions, one supported by a 24-inch waffle slab. “There was a lot of upfront capital cost involved, but that gave Emory the flexibility to house some other pieces of equipment in the future,” says Mistry.
A Game of Inches—And Tons
In the end, the planning paid off. The 10-foot-wide corridor was able to accommodate the 60,000-pound 7-Tesla MRI, with 2 inches to spare.
Some of the equipment required various hook-ups immediately after arrival. One vendor told Mistry that its machine “needed life support. It needs a minimum of cooling, data, and other things that need to be active 24/7. Otherwise, the equipment is going to die,” says Mistry.
Most machines were moved in without any trouble. However, despite all that careful planning, a few things still went wrong. One completed floor needed to have some rebar removed, because a vendor forgot to inform Emory about their equipment’s magnetic tolerances. Another piece of equipment stopped working within three months of installation and had to be replaced. Budgets were also subject to sudden strains. In March 2021, for instance, after a cargo ship became stuck in the Suez Canal, cargo rates went through the roof, making it much more expensive to get equipment manufactured in Europe shipped to Atlanta.
But even as they build a new facility, core facility architects already need to think about how they take the machines out, when today’s cutting-edge equipment will become outdated. “Because these are big pieces of equipment that you have to put in and then build the building around, how would you take it out, say, 10 years from now?” says Mistry.
The general trend in advanced medical and scientific equipment is for it to become smaller even as its capabilities multiply, according to Mistry. But he believes that won’t make things any easier for architects, because even as the machines’ spatial needs shrink, their infrastructure requirements are likely to grow.
By Bennett Voyles